Choosing Whether or Not to Menstruate
The average woman spends roughly six years of her life menstruating. Most of us just accept this as part of life, but it would be really nice not to have to worry about it.
The miracles of modern science have given us several ways of doing just that. We are able to alter how our bodies function at a fundamental level, although it takes a little more effort than just waving a magic wand. There are safety concerns to take into consideration.
Why would someone want to get rid of their period?
Although menstruating is a natural process, for some women is it so debilitating that they are forced to put their lives on hold. Even women who suffer less lead busy lives, so dealing with cramping, headaches, and blood is not a welcome. It is not uncommon to wish that it would just stop.
Many women have no wish to have children and are confident this will not change in the future. For them, going through a process that prepares their bodies for the chance of pregnancy can seem completely unnecessary.
Hormonal contraceptives
Hormones are integral to the menstrual cycle. Hormonal birth control acts on the female endocrine system to prevent pregnancy. This is achieved by thickening the cervical mucus to keep sperm from entering the uterus, by thinning the uterine lining to prevent the implantation of a fertilized egg cell, by preventing eggs from being released in the first place—or some combination of the above.
There are two widely accepted ways of categorising hormonal contraceptives:
- Time-frame for renewal? short-acting reversible contraceptives (SARCs) and long-acting reversible contraceptives (LARCs)
- Ingredients: progestin-only contraceptives (containing, as the name implies, progestin only) and combination contraceptives (which contain both progestin and oestrogen).
These distinctions are important not only because they contain relevant information about how to use the type of birth control you have chosen, but also because there are a number of health conditions that react dangerously to oestrogen.
Combination contraceptives can cause complications if you are pregnant or in the first month of breast-feeding, and if you are obese, a smoker or recent smoker over the age of 35, have a history of blood clots, thrombosis, stroke, heart problems, cancer, liver or gallbladder disease, diabetes or related complications, severe migraines (especially with an aura as a warning sign), or are taking any medications that may interact with birth control (this includes certain antibiotics).
Even taking contraceptives correctly is not always a walk in the park. Typical possible side effects of taking hormonal birth control include weight gain, headaches, sore breasts, irregular periods, mood changes, decreased sexual desire, acne, and nausea. These vary from person to person, and sometimes are simply a sign of your body adjusting to the contraceptives.
No matter the type of hormonal contraceptives you plan on taking, always consult a qualified professional about possible risks beforehand. Even if you cannot think of anything that might go wrong, there is always a chance you are unaware of some key bits of information.
The contraceptive pill
‘The pill’ is a SARC. It is used selectively to create an artificial menstrual cycle. This is achieved by taking a set of ‘active’ pills containing hormones that keep you from menstruating, followed by a set of ‘inactive’ pills that do not contain hormones or simply taking a break from the pills, which allows the uterine lining to shed.
Most SARCs follow a 28-day cycle (the average of natural menstrual cycles). This means you take hormones for 21 days and then stop for 7 days. There are also extended-cycle pills, which are taken continuously for 12 weeks, followed by one week of inactive pills, reducing the number of menstrual periods from an average of 13 per year to 4 per year.
You can eliminate this artificial period simply by skipping the inactive pills and starting the next set of active pills. Your uterine lining will not break down and shed, so you won’t bleed. If the pills are taken correctly, there should be no adverse effects. The possible side effects of taking the pill continuously for several months are the same as when following the 28-day cycle. Hormone levels remain constant, meaning no endometrial build up in the uterus. In fact, the longer you take the pill, the thinner the lining of the uterus becomes. However, it will return to normal once you stop taking the pill.
Some women experience spotting (a small amount of bleeding between periods) when they start taking the pill continuously. This usually disappears over time as the body grows accustomed to the change. Others may start spotting after a few months, in which case they take the inactive pills and have their period.
Injections
Contraceptive injections are LARCs. They work by suppressing ovulation, preventing the ovaries from releasing an egg. They also thicken the cervical mucus to prevent the sperm from reaching the egg.
There are four main types of birth control shots—Depo-Provera (DMPA), Combined Injectable Contraceptives (CICs), Sayana Press, and Noristetat (NETE). The availability of these differs from country to country. All types of injections are 99% effective when used properly. The main differences are injection site, length of effectiveness, and time needed to regain fertility.
While many women stop getting periods after the first couple of injections, this is not true for everyone. Your periods can change, becoming either heavier or lighter, or may stop altogether. Cessation of menstruation is not the goal of an LARC injection, but rather a side-effect. This means that it is not a sure-fire way to stop bleeding.
That being said, 60–70% of women who start using LARC injections stop having periods, but it usually takes up to a year for the periods to fully stop.
The hormonal IUD
The IUD (or intrauterine device) is a small device that is inserted into the uterus to prevent pregnancy. It is also an LARC, and one of the most effective birth control methods. The hormonal IUD releases a form of progestin that thickens the cervical mucus so that sperm can't reach the egg. In some women, progestin may also prevent ovulation. There is also a non-hormonal IUD that does not affect hormone production.
Some women experience longer and more painful menstrual periods in the first 3–6 months after having an IUD fitted. There is some risk of infection and of the body rejecting the device—your doctor will let you know how to check if it’s in place. The IUD is not recommended for women who have a history of pelvic infection. The hormonal IUD can stay in place for 3 to 5 years, depending on the brand.
Hysterectomy
A hysterectomy is surgical removal of the uterus or womb and sometimes other surrounding structures.
The removal of the uterus, ovaries, or fallopian tubes renders patients infertile, ceasing menstruation. The surgery comes with some risk and is usually recommended only if other treatments have failed or are not possible.
Hysterectomy is used to treat problems affecting the female reproductive system, including:
- endometriosis
- chronic pelvic pain
- heavy menstrual bleeding
- uterine fibroids
- gynaecological cancer
There are three types of hysterectomies:
- Total hysterectomy: the removal of the womb and cervix
- Subtotal hysterectomy: the removal of the main body of the womb, leaving the cervix in place
- Radical hysterectomy: the complete removal of the uterus, cervix, upper vagina, and parametrium. This procedure is usually performed as a treatment for cancer.
A number of surgical approaches can be used to perform a hysterectomy. Each has advantages and disadvantages. Your doctor will determine which type of hysterectomy is best suited for your situation.
While the procedure is generally considered safe, the following problems can occur in rare cases: urinary incontinence (involuntary leakage of urine), vaginal prolapse (a condition where the vagina moves out of place), the formation of a vaginal fistula (an abnormal connection that forms between the vagina and another organ), chronic pain, heavy bleeding, blood clots, haemorrhages, injury to surrounding organs, and infections.
After a successful hysterectomy, the patient is required to stay in the hospital for up to 5 days and is expected to make a full recovery in 6 to 8 weeks. Recovery times differ depending on procedure.
No blood, no problem?
Wanting to live a life without periods is completely understandable and possible, however there is a lot to consider when making these choices. Sometimes the problem isn't actually the period itself, but rather the symptoms that accompany it.
Depending on what it is that you want to get rid of, it might be worth looking into less body-altering options. In some cases, the change could be as small as reducing stress in your day-to-day or limiting your intake of any foods or substances that may be affecting your body.
That being said, if you are suffering you should feel free to take any action that you feel is needed, as long as you are not putting yourself in harm's way and are informed about your choices. It is your body, after all.
A note from the editor: Due to the amount of overlapping information, we quote from our article on Hormonal Birth Control.
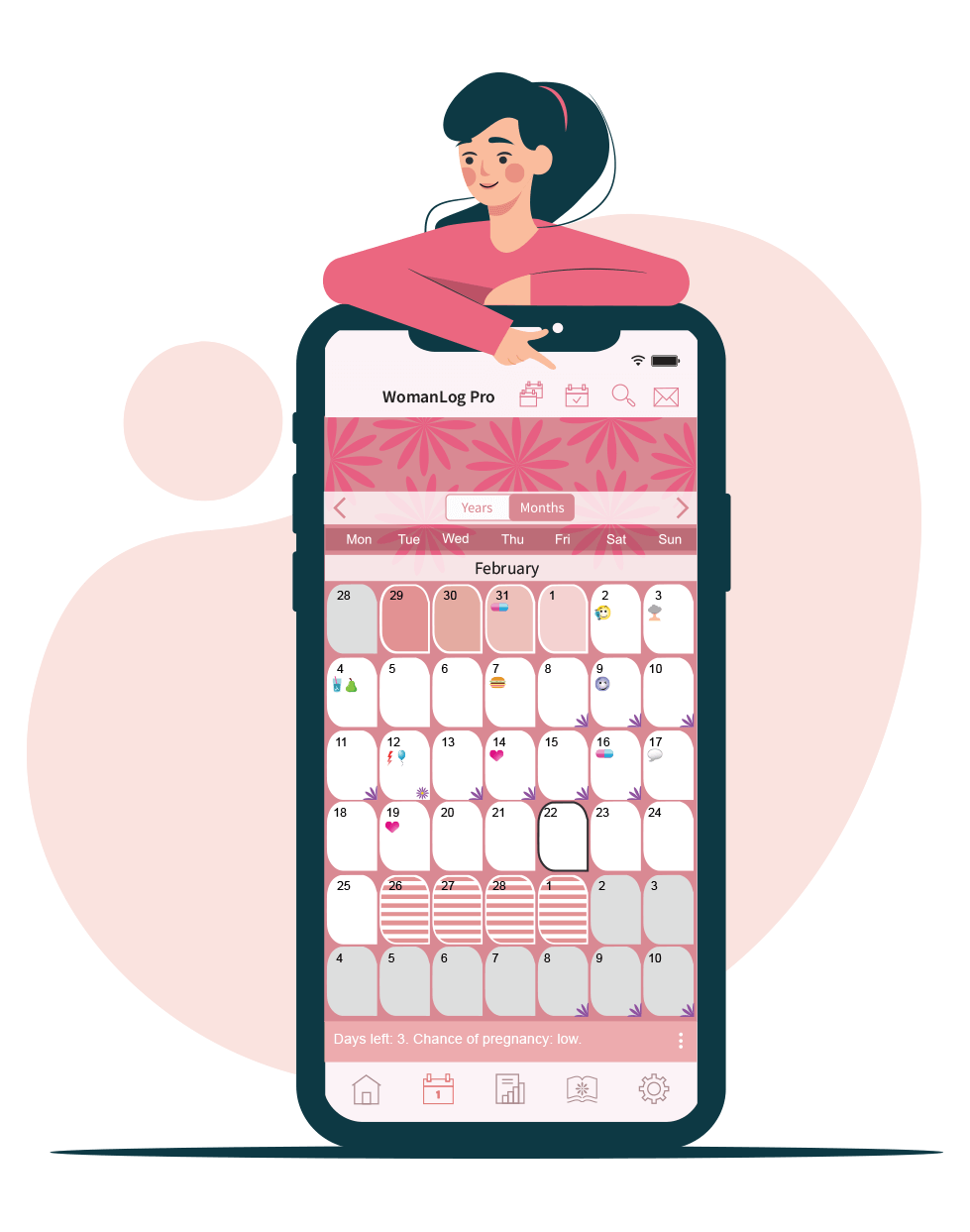
You can track your period using WomanLog. Download WomanLog now: