Permanent Birth Control for Women
The only sure method of birth control is abstinence, they say. While it’s true that if you never have sex, you cannot become pregnant, there are several methods of surgical contraception, or sterilization, that are also nearly 100% effective. What are they and why is this topic so heavily stigmatized?
We don’t often talk about voluntary sterilization because it is a serious step and, in many cultures, motherhood is seen as a biological imperative for women so choosing to go against that expectation can be stigmatizing. The consequences of voluntary sterilization and the difficulty of the procedures involved for men and women can be quite different.
The sterilization procedure for men is the vasectomy—the cutting and sealing of the vas deferens or sperm duct; this procedure is quick, minimally invasive, and can often—but not always—be reversed. The tubal ligation procedure for women is riskier and more complicated, and although in some cases it may be reversible, that would involve major surgery and is rarely fully successful, so the decision to undergo a tubal ligation should be considered final.
Whenever someone engages in sexual activity with a person of the opposite biological sex there is always the chance of getting pregnant. Depending on your definition, even “abstinence” may not be 100% effective in preventing pregnancy if, for example, you abstain only from penis-in-vagina sex but engage in other types of sexual activity.
Although it happens rarely, pregnancy has been known to begin even from traces of sperm, for example, on the thigh that, under the right conditions, can still manage to fertilize an egg. Small amounts of sperm are also present in pre-cum. According to the US Center for Disease Control, “pulling out” fails to prevent pregnancy 22% of the time: that's more than 1 out of every 5 times, statistically!
While unintended pregnancy is common among both partnered and single women, it is almost twice as common among single women who are at the beginning or near the end of their reproductive years.
Resolving an unintended pregnancy through abortion is associated with medical and psychological risks, and in some countries this choice carries negative political/legal consequences. In June of 2022 the US Supreme Court overturned a ruling that had been in force for 50 years granting the right to abortion. Access to abortion has now been banned or severely limited in 26 states and there is an ongoing effort to ban abortion nationwide.
Regular Vs Permanent birth control
Most people use birth control so they can enjoy sex without the fear of becoming responsible for offspring they are not prepared to care for. You can read about various methods of birth control, both hormonal and non-hormonal, and their varying success rates in our previous articles. Such contraceptives are used in the moment or month-to-month, as well as on the morning after. Once you stop using them, the possibility of getting pregnant returns.
Sterilization, on the other hand, is permanent, and the practice is stigmatized; although less so now than in previous decades. A woman who voluntarily chooses this method of birth control tends to be judged negatively by others, may be seen as less warm, and may evoke “passive harm behaviours” such as avoidance, envy, or disgust.
If you are considering sterilization, be prepared for pushback from friends and family and for the potential that the medical professionals you consult may also harbour negative preconceptions about your choice.
Reasons for voluntary sterilization
As sterilization in women is almost always permanent, the biggest concern for practitioners is that this choice should not be made for wrong reasons, which can cause feelings of deep regret down the road. According to a study done in 2012, women were more likely to regret their sterilization if they were young, had few or no children, were pressured by a partner, or thought sterilization would help them fix financial or relationship problems.
Doctors are more likely to reject a request for voluntary sterilization if you are under 30, or even 35, or have never given birth. You will likely have to answer a number of probing questions and be asked to sign an informed consent form before the surgery. Attitudes are changing, but in some places outdated, misogynistic attempts to control women’s bodies are still very much the reality.
Permanent birth control, or voluntary sterilization is a deeply personal choice and is recommended only if you are absolutely certain you will not wish to have children in the future. This decision must be yours and it should never be influenced by the opinions of your partner, family members, friends, or anyone else. The people around us may change but we only get one body.
Sometimes, a gynaecological condition such as cancer of the cervix or some other part of the reproductive system requires surgical intervention that results in sterilization. In such cases the responsible surgeon will inform you of your options and ask for your consent before the surgery is performed.
Likewise, sterilization can be an option after giving birth through a Caesarian section. Again, only with your informed consent. It is sometimes recommended after especially difficult births where it is clear that the issues would return with any potential future pregnancies or performed on the mother's request.
Regrettably, in the past, sterilization has at times been forced on people belonging to a race or nationality, or any other group of people considered less worthy or desirable, for example, on the basis of disability. Sometimes this force has been direct and physical, ordered by law and forced on people. Other times it has been indirect—using political pressure or misrepresentation, suggesting that people "make this choice" for themselves.
Involuntary sterilization has done significant and lasting harm to certain communities that continue to suffer the consequences to this day. According to some reports, this practice might still be used in certain places. Such targeted sterilization is considered a form of genocide, and not something to be taken lightly.
Tubal ligation
The most commonly available type of permanent birth control for women is tubal ligation, or “getting your tubes tied”. This method is more than 99% effective in preventing pregnancy.
What is tubal ligation? Fertilization typically takes place during or shortly after intercourse in the fallopian tubes when an egg that has been released (by one or the other ovary) and is making its way toward the uterus meets sperm travelling up the vaginal canal. Tubal ligation is a surgical procedure performed under general or local anaesthesia during which the surgeon seals off the fallopian tubes.
In some cases, a small section of each tube is excised, or the fallopian tubes may be removed entirely. This procedure is usually performed laparoscopically—through a small incision made near the belly button or in the lower abdomen.
Where does the egg go after tubal ligation? Your ovaries continue to produce eggs in accordance with your menstrual cycle and your period continues as usual. However, as the egg is unable to travel through the fallopian tubes to the uterus, it is reabsorbed into the body each month instead of flowing out with the menses.
How effective is tubal ligation? Tubal ligation is more than 99% effective in preventing pregnancy. Research shows that only 2–10 of every 1000 women who have undergone tubal ligation become pregnant after the procedure.
What are the risks? As with any surgical procedure there is a risk of infection; of damage to nearby internal organs, such as the bladder; of an adverse reaction to the anaesthesia used; and of post-surgery trauma, among other potential problems.
On rare occasions, a sperm might still find its way to an egg, and if this does happen there is heightened risk of ectopic pregnancy, when the fertilized egg does not reach the main part of the uterus but implants elsewhere, usually in the fallopian tubes.
Tubal ligation is not recommended for people with:
- diabetes;
- lung disease;
- obesity;
- pelvic inflammatory disease.
Of course, there is also the psychological risk for any type of permanent birth control: the potential for regret if the now sterile person changes their mind in the future and wishes to become pregnant after all. Procreation as part of the human experience is a very deep and still unexplored phenomenon, sometimes it is impossible to predict our own feelings about the subject matter when placed in situations where it is concerned.
Apart from tubal ligation, there is another option for women that completely prevents the chance of pregnancy, but it is generally not offered as a form of birth control by choice.
Hysterectomy
Hysterectomy is another surgical procedure that results in sterilization. In this case the uterus is removed—either by itself or together with other female reproductive organs such as the cervix, the fallopian tubes, and the ovaries. Not having a uterus completely eliminates the possibility of pregnancy. Under certain, very rare conditions, an ectopic pregnancy may still occur, but could never be carried to term.
Hysterectomies are not typically considered a form of birth control. This surgery may be performed in the case of:
- ovarian, uterine, or cervical cancer;
- other types of cancer within or near the reproductive organs;
- uterine fibroids (non-cancerous growths);
- extremely heavy periods;
- strong cervical pain;
- endometriosis;
- strong bacterial infections in the reproductive organs;
- health conditions preventing the possibility of a healthy pregnancy
Post-partum hysterectomies
Post-partum hysterectomies are sometimes performed when the mother's health or life is in danger due to emergencies during labour or other complications. In this case, the womb is removed during the C-section or in the 24 hours after giving birth. It can also be a pre-planned part of the Caesarian section to prevent future pregnancies.
Your reproductive health journey still continues
Remember, having safe sex is not just about birth control! If you go through with permanent birth control, you should still protect yourself against STIs by using a condom or other protective barrier.
Likewise, if you still have your cervix and other reproductive organs, you still need to do smear tests and regular check-ins with your OB/GYN to monitor your health.
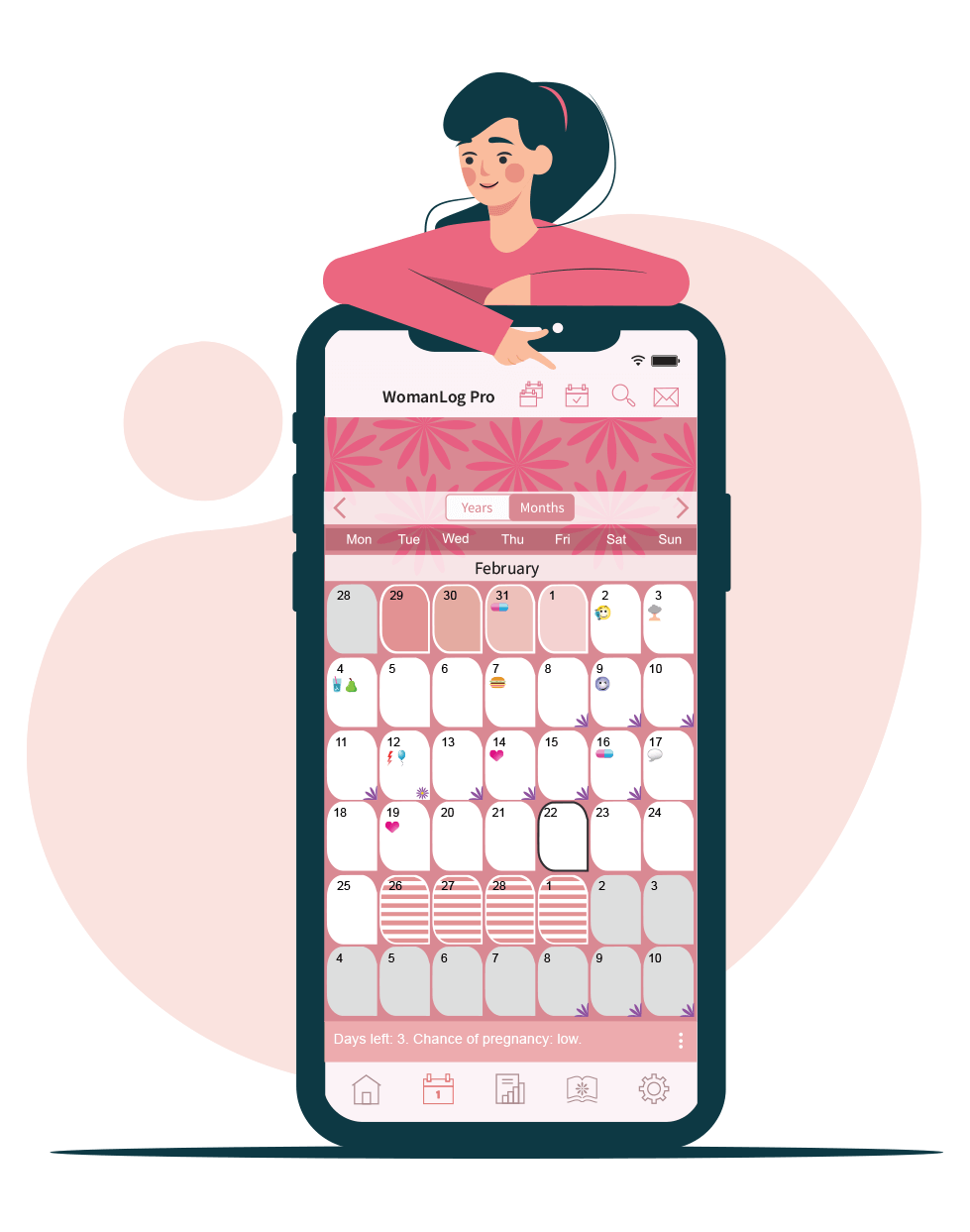
Download WomanLog now: