Contraception For Men
Safe contraception should be available to everyone. Access to contraception allows us to plan for pregnancy, protect ourselves from sexually transmitted infections (STIs), and gives us more control over our lives.
Most sexually active people who aren’t planning to get pregnant use some method of birth control. Birth control, or contraceptives, is our primary means of reducing unwanted pregnancies (and therefore abortions) and protecting against STIs. However, women shoulder an unfair share of the responsibility for preventing pregnancy. In this article, we provide a brief overview of the different types of contraception, discuss the options available for men, and consider what can be done so partners can share the responsibility equally and enjoy safe sex.
How many types of contraception are there?
There are many methods of birth control available to people of all ages. These are typically classified as hormonal or non-hormonal.
Hormonal birth control methods are designed for women and come in a variety of forms—the pill (taken daily), the patch (applied weekly), the shot (lasts 3 months), the vaginal ring (lasts 3 months), the implant (lasts 3 years), and the hormone IUD (lasts 3–10 years). Hormonal contraceptives temporarily alter the natural menstrual cycle by releasing synthetic hormones into the bloodstream that thicken the cervical mucus, making it difficult for sperm to enter the uterus and prevent ovulation, so there is no egg to fertilise.
There’s a common misconception that a woman can get pregnant any time of her cycle, but this is not true. The menstrual cycle has three phases—the follicular phase, the ovulatory phase, and the luteal phase. A woman can become pregnant only during the ovulatory phase, which occurs in roughly the middle of the monthly cycle and lasts 24 to 48 hours. This is the time when one of the two female ovaries releases a mature egg into the corresponding fallopian tube so it can make it’s way to the uterus. If sperm is present in the uterus at that time, the egg may be fertilised. If so, it will implant into the uterine wall, where it will begin to develop.
Follow this link to read more about The Monthly Cycle.
Hormonal birth control is popular because it’s 99% effective, the effects disappear once the synthetic hormones leave the body, and they require little or no maintenance. While this seems to be an ideal solution to birth control, hormonal contraceptives do not protect against sexually transmitted diseases, and some women experience detrimental side effects including headaches, weight gain, mood changes, sore breasts, vaginal irritation, irregular bleeding, changes in libido, acne, and nausea. Long-term use of hormonal birth control slightly increases a woman’s risk of developing blood clots and having a heart attack. Many women have no trouble using hormonal contraceptives. For those who are concerned about the possible side effects, other options are available.
Read next: What to Expect When You Stop Taking Hormonal Birth Control?
Non-hormonal birth control methods include various types of barriers, the copper (non-hormonal)IUD, spermicide, fertility awareness, withdrawal, and permanent sterilisation.
Barrier methods designed for women include the diaphragm, the cervical cap, the sponge, and the female condom. When used correctly, these methods are also quite effective (~95%) and can be used in combination with spermicide to improve their effectiveness.
Spermicide can also be used by itself, but then it is only about 70% effective. It is sold as foam, jelly, cream, dissolvable film, or in tablet or suppository form. Nonoxynol-9 is a common spermicide and the only type that can legally be sold in the US. Most spermicides are surfactants, or surface-active agents, which disrupt the surface membrane of the sperm; this slows the sperm down and eventually destroys them. Spermicide must be inserted into the vagina 10–15 minutes before intercourse and remains effective for up to 3 hours. Some condoms and all contraceptive sponges are coated in spermicide. The substance can cause irritation and increase the chances of contracting an STI in some cases.
A newer type of spermicide, branded as Phexxi, is a non-hormonal gel that alters the pH of the vagina, making it inhospitable to sperm. This is said to be 93% effective but is relatively expensive and available only with a prescription. Like Nonoxynol-9, it can also cause mild to moderate side-effects such as burning, itching, discharge, infection, and bacterial vaginosis in some people.
An all-natural method of birth control is the fertility awareness method. Women who choose this path track their menstrual cycle and accompanying bodily changes. By learning about how vaginal fluids and body temperature change in reaction to fluctuations in the reproductive hormones, a woman can become quite good at predicting when she is in the ovulatory phase of her cycle and use this knowledge to avoid pregnancy or to maximise her chances of getting pregnant.
If a couple has had unprotected sex or their birth control has failed for some reason, the woman has a short window of time—72 to 120 hours—when she can use an emergency contraceptive pill that delays ovulation to avoid pregnancy. If fertilisation and implantation have already occurred, the pill will not be effective. These pills can cause some nausea, vomiting, headaches, and tenderness in the breasts, but these effects are usually minor and subside in a day or two.
The most radical type of birth control is sterilisation. In women, this generally means a tubal ligation, and in men, this means a vasectomy. (More details below.) While in some cases, these procedures can be reversed, they are generally considered permanent and should only be performed on people who are quite sure they will not want biological children of their own in the future.
Types of contraception available to men
As you can see, there are many types of contraceptives designed for women, but men have more limited options. Apart from abstinence and the questionable “withdrawal method”, men have only two options for active birth control—use condoms or get a vasectomy.
Condoms have been used to prevent unwanted pregnancies for at least several hundred years and perhaps even longer. Although the materials and reliability have been upgraded, the basic design of the condom remains unchanged. Condoms are still a primary method of birth control in our time, and to this day, they are the only reliable method of preventing STIs, including HIV.
The Condom
A condom is a thin sheath, most commonly made from latex rubber that a man unrolls over his erect penis. Once securely in place, the condom acts as a barrier, blocking the sperm a man ejaculates during intercourse from entering the vagina of his sexual partner. When stored and used properly, latex condoms are highly effective in preventing pregnancies and STIs.
As some people are allergic to latex, condoms are also made from polyisoprene—a synthetic rubber that behaves much like latex, polyurethane—a thin plastic that is less stretchy than rubber and so a little more likely to slip off, and “natural lambskin”—actually the cecum or membrane at the start of the large intestine. Condoms made from membranes have been used for thousands of years. Some people find that lambskin condoms feel more natural and enhance sensation, but while they are effective at blocking sperm, the pores are too large to prevent the transmission of many STIs. Such condoms are also significantly more expensive and are packaged in an antiseptic fluid that has a slight odour some find unpleasant.
Condoms should be stored safely, away from sharp objects, at a temperature between 0° and 38° Celsius (32° and 100.4°F). Your wallet is not a good place to store condoms.
Condoms come in a wide variety of colours; they may be smooth or textured for extra sensation, and some are even scented or flavoured. Most have a ‘reservoir tip’ where the ejaculate can collect. They are packaged in lubricated wrappers, sometimes including spermicide. Many people like to use some additional lubrication to avoid friction. Water- and silicone-based lubricants are good choices for use with latex and polyisoprene condoms. Oils damage rubber, so oil-based lubricants such as massage or baby oil, lotion, or petroleum jelly are only safe to use with polyurethane or lambskin condoms.
To avoid contracting or passing on an STI, a condom should be worn during vaginal, anal, and oral sex. When used with care, condoms are 98% effective in preventing pregnancies; when used with typical haste, they are effective 85% of the time.
Vasectomy
A vasectomy is a minimally invasive surgical procedure, requiring only a local anaesthetic, in which the vas deferentia—the ducts that convey sperm from the testicles to the urethra—are cut and sealed; it can be usually completed in 20–30 minutes, and sexual intercourse can often be resumed with little discomfort in about a week. However, millions of sperm remain in the tubes above the incision sites, and it requires about 25 ejaculations to clear them from the body. During this time, another form of contraception must be used.
The corresponding procedure for women is a tubal ligation (having your “tubes tied”) in which the fallopian tubes are cut, blocked, or removed. This is a more invasive procedure that requires access through the abdomen, so regional or general anaesthesia is required. Women who undergo tubal ligation experience few or no changes in their menstrual cycle, the age of menopause does not appear to be affected, and sexual function is unchanged or even slightly improved. However, women who have had tubal ligation surgeries are four to five times more likely to undergo hysterectomy (removal of the uterus) later in life than those whose partners underwent a vasectomy. The reason for this is unknown. Hysterectomy and bilateral oophorectomy (removal of both ovaries) also result in sterilisation, but these surgeries are more invasive and carry greater health risks.
Internationally, vasectomy rates differ greatly, with men in developed countries being much more likely to undergo the procedure than men in the least developed countries. For example, 22% in Canada vs 0,3% in Swaziland. Some men believe that an inability to father children is emasculating, but this is not true. Five to ten times more women worldwide have undergone sterilisation than men, even though the procedure for women is riskier and more complicated. Some people, especially those under the age of 30, experience regret after sterilisation, but the majority are happy with their decision, especially committed partners who have made the decision together.
The Withdrawal Method
Withdrawing the penis from the vagina right before ejaculation can also be considered a type of contraception. If done correctly, this prevents sperm from reaching the female reproductive organs and it can be up to 94% effective. For this method to work, partners need to work together, and the man must have the self-control to pull out before reaching orgasm. Even if you do everything right, pre-ejaculation fluid might get inside the vagina and contain enough sperm for this to result in pregnancy. That’s why it’s effective only 78% of the time with typical use. The withdrawal method also doesn’t prevent sexually transmitted infections.
Other Potential Options for Male Contraceptives
Since the 1970s, there have been a number of attempts to create male contraceptives, but so far none are available on the open market.
Intra-vas Injections
The RISUG (reversible inhibition of sperm under guidance) shot is non-hormonal, minimally invasive, and reversible. A positively charged polymer gel is injected into the vas deferens, where it attaches to the walls. When negatively charged sperm pass by, it damages their heads and tails, making them infertile. An injection of water and baking soda can be used to flush the gel from the ducts, restoring fertility with no side effects. Another similar injection under the name Vasalgel works by forming a hydrogel that blocks the vas deferens instead; it can also be flushed from the body to restore fertility. Both are still under development for humans.
Hormonal Contraceptives
Androgens (steroid hormones) have been shown to reduce sperm count without affecting the male sex drive or the ability to achieve orgasm. Testosterone injections suppress follicle-stimulating hormone (FSH—a hormone that controls sperm production) and luteinising hormone (LH—a hormone that regulates testosterone in men), reducing the number of sperm in the testes. A number of trials have been conducted using this principle.
Non-hormonal Contraceptive Pills for Men
Gendarussa is a contraceptive that has been available in Indonesia through clinical trials since the 1990s; its active ingredient is derived from the Justicia gendarussa plant and works by interfering with an enzyme in the head of the sperm, making them unable to penetrate the egg. An Epididymal Protease Inhibitor has shown promising results in animal studies; it works by binding to a protein on the sperm’s surface to keep it from swimming. The Clean Sheets Pill was another exciting project that received a lot of attention in England around 2012. Not only did it allow men to achieve orgasm without ejaculating, but it also reduced the transmissibility of HIV in semen. The pill works by relaxing the longitudinal muscles along the ducts that carry the sperm from the testes while not affecting the circular muscles that clamp down on them or inhibiting orgasm in any way. The pill must be ingested 2–3 before sex, and the effects wear off 16–24 hours later. Unfortunately, the project stalled due to a lack of funding.
Why it’s important to share the responsibility
Whenever a man and a woman engage in sexual intercourse, they create the potential for bringing another human being into the world. The responsibility for regulating this process has traditionally been placed on women. It is up to the woman who becomes pregnant to carry the child to term, give birth, and care for it in infancy, so it is also up to her to refuse sex if she doesn’t want to risk pregnancy or control her own fertility.
The first oral contraceptives for women became available more than 60 years ago. Providing a reliable method of regulating fertility sparked a sexual revolution that empowered women and gave them the ability to enjoy sex without fear and the right to choose when and if they wanted to bear children. This type of freedom for women is not without political consequences and is not welcomed everywhere in the world. However, for the first time in several generations, women’s rights to contraceptives and to legal abortion are under attack in the US.
To this day, many women are left alone with the responsibility of unwanted pregnancy because birth control failed. When men take an active role in birth control, not only does the number of unwanted pregnancies and abortions decrease, but their female partners are more likely to feel safe and supported. While condoms are still important in preventing STIs, giving men more contraceptive options would give them greater control over their bodies and allow them more freedom to decide when and if to have children. The trend among young people today is toward fewer and more stable relationships than was common for their parents, and shared responsibility for birth control is part of that trend.
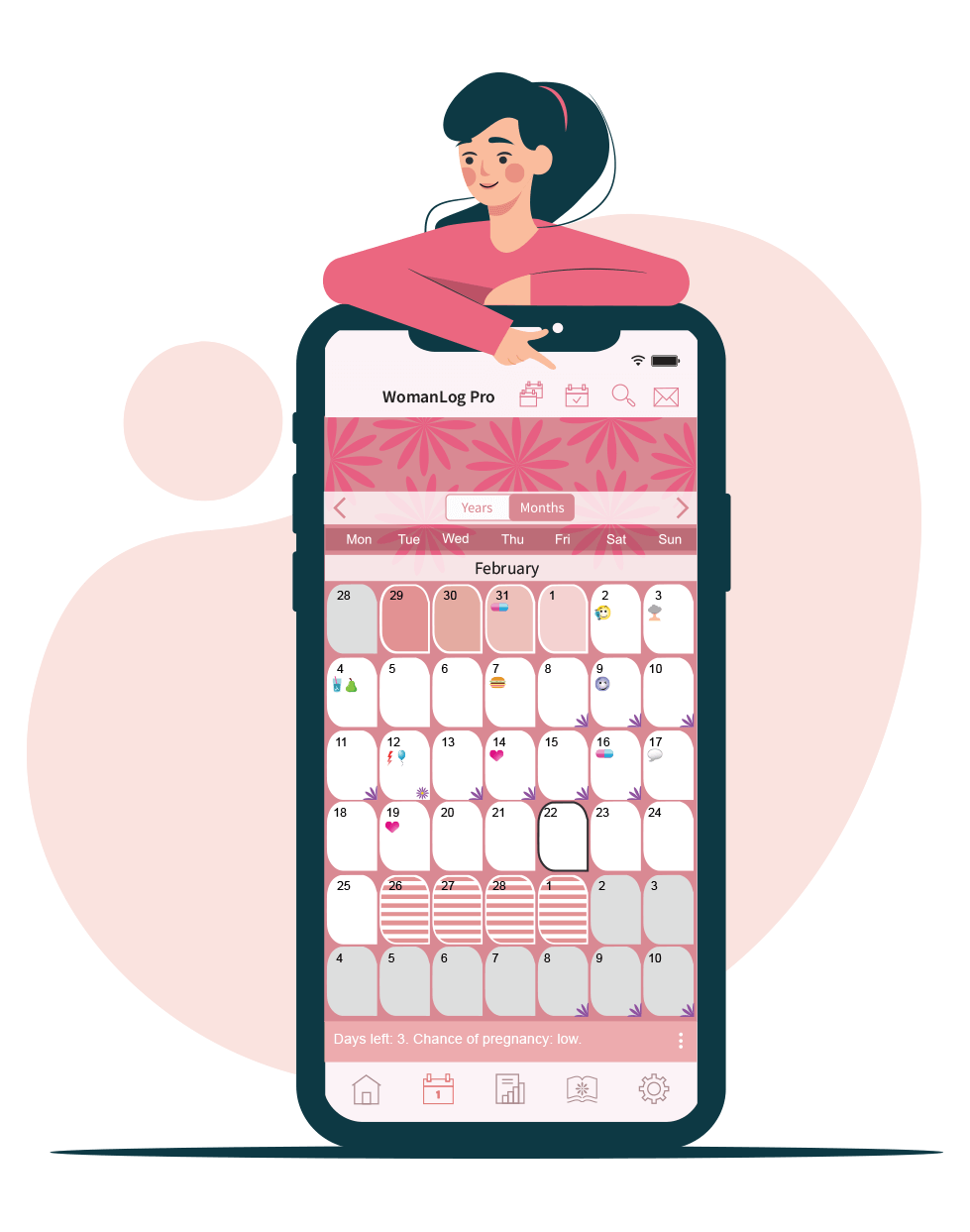
You can track your period using WomanLog. Download WomanLog now: