Hormonal Birth Control
Taking charge of our menstrual cycles can be empowering—knowing when to expect periods and reducing or even eliminating accompanying symptoms makes it much easier to manage, and frees up time and energy to use as we see fit!
All hormonal contraceptives contain a small amount of synthetic estrogen together with progestin (a form of progesterone), or progestin alone. These hormones work to inhibit the body's natural analogue hormones.
Hormonal birth control acts on the endocrine system to make the body prevent pregnancy by thickening the cervical mucus to keep sperm from entering the uterus, by thinning the uterine lining to prevent the implantation of a fertilized egg cell, or by preventing eggs from being released in the first place—or some combination of the above.
Do not take hormonal birth control if you are pregnant, obese, a smoker or recent smoker over 35, or are taking any medications that may interact with birth control. Hormonal birth control is also not recommended if you have a history of blood clots, thrombosis, stroke, heart problems, cancer, liver or gallbladder disease, diabetes, or severe migraines (especially with an aura as a warning sign). If you are considering this method of contraception consult your doctor about possible risks.
Short-acting reversible contraceptives
SARCs are ingested or applied daily, weekly, or monthly, depending on the method.
The pill, or combined oral contraceptive pill, inhibits the menstrual period, and is therefore taken selectively to create an “artificial” menstrual cycle.
- Monophasic 21-day pills each contain the same amount of hormones. They are taken once every day for 21 days, and then not taken for a week so the menstrual period may happen.
- Phasic 21-day pills have two or three kinds of different coloured pills containing different amounts of hormones. These need to be taken in order, once every day for 21 days, and then not taken for a week.
- Every day pill sets have 21 “active” pills that contain hormones, and 7 “inactive” pills that do not—28 pills in total. This allows your period to take place without interrupting the daily ritual of taking a pill at a certain time. These must also be taken in the right order to be effective.
- Extended-cycle pills are taken continuously for 12 weeks, followed by one week of inactive pills. This reduces the number of menstrual periods from an average of 13 per year to 4 per year.
Mini-pills are taken daily and contain only progestin. Women who experience side-effects from contraceptives containing estrogen may fare better with mini-pills.
Breastfeeding women are advised to opt for progestin-only birth control instead of pills containing both estrogen and progestin, as estrogen can adversely affect milk production. However, specialists recommend non-hormonal contraceptives (such as condoms or the LAM method) as a first choice.
If mini-pills are used consistently and correctly, they are about 95% effective—slightly less effective than standard birth control pills.
The vaginal ring is a small plastic ring that sits inside the vagina and releases estrogen and progestin into the bloodstream. Like the pill, it is used for 21 days, then taken out for 7 days, after which a new ring is inserted.
The skin patch is placed on the abdomen, buttocks, upper arm, or upper body (not the breasts); once in place it releases a regular dose of estrogen and progestin. When used correctly, it is >99% effective.
A woman changes the patch once a week for 3 weeks and then goes without a patch for 1 week. During the week without the patch, she may experience light menstrual bleeding. The skin patch can be worn in the bath, while swimming, and while playing sports.
The patch can raise your blood pressure, and some women experience temporary side effects such as headaches, mood changes, lower libido, or weight gain.
Long-acting reversible contraceptives
LARCs can last weeks, months, even years, demanding relatively little monitoring or upkeep.
The birth control shot contains progestin only. It is injected every 8–13 weeks, depending on the brand. Many women stop getting periods after the first couple of injections. If injections are discontinued, the progestin will dissipate over time. Most women start having periods and become fertile again 4 to 8 months after their last injection, but it can take longer for some.
The contraceptive implant or birth control implant is a rod about the size of a matchstick that is inserted under the skin of a woman’s upper arm and releases progestogen into the bloodstream. This steroid hormone binds to and activates the progesterone receptor. The implant becomes effective 5 days after insertion and the effects last 3–5 years. After the implant is removed, chances of pregnancy return. The affected arm may be tender or swollen for a few days, but there should be no other noticeable after-effects. Benefits include fewer and lighter periods, milder PMS symptoms, and it is smoker- and breastfeeding-safe.
The hormonal IUD or intrauterine device is a T-shaped device that rests inside the uterus and releases a form of progestin. The progestin thickens the cervical mucus so that sperm can't reach the egg. In some women, progestin may also prevent ovulation. The IUD is effective immediately and can last for 5–10 years, depending on type. After removal, chances of getting pregnant return right away.
Some women experience longer and more painful menstrual periods in the first 3–6 months after having an IUD fitted. There is some risk of infection, and of your body rejecting the device—your doctor will let you know how to check if it’s in place. The IUD is not recommended for women who have a history of pelvic infection.
Attention! Hormonal contraceptives can have serious side effects and can heighten the risk of venous thromboembolism, stroke, myocardial infarction, and some cancers. If you experience abdominal or stomach pain, severe headaches or migraines, shortness of breath, chest pain, blurred vision, or redness, swelling, or pain in the legs after starting hormonal birth control, visit your doctor immediately!
Emergency contraception
The morning-after pill is meant to be used after unprotected sex or protected sex with compromised primary birth control, such as a torn condom. It must be taken within 5 days after unprotected sexual intercourse—the sooner, the better. This method is for emergency situations only and should not be used as regular birth control.
The IUD can also be used as emergency contraception, also up to 5 days after sex, and is in fact considered more effective than the morning-after pill.
There is still some stigma surrounding birth control, but don’t let that stop you from giving yourself all the tools you need to lead a full life.
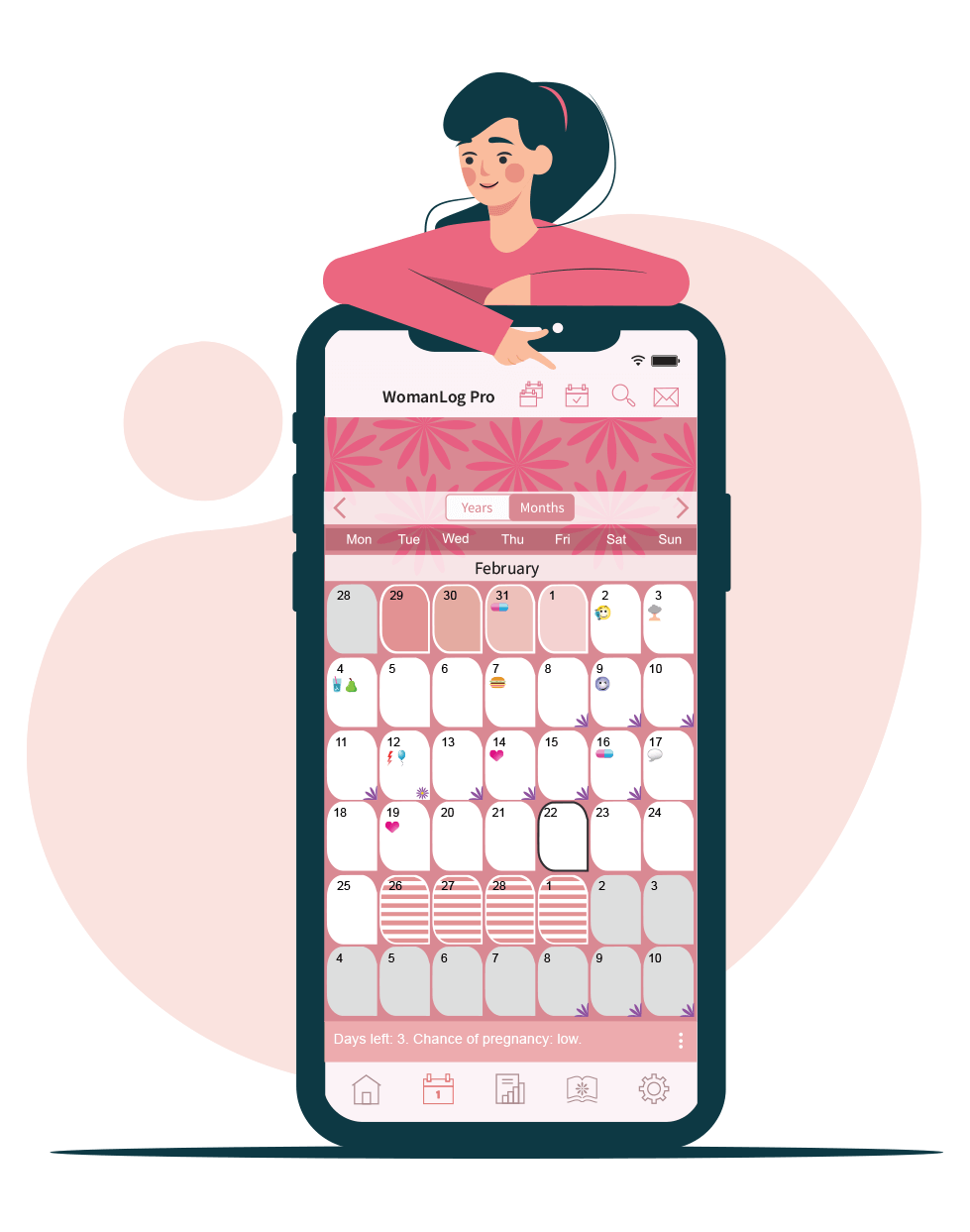
You can set reminders for birth control methods using WomanLog. Download WomanLog now: