Premenstrual syndrome (PMS)
Headaches. Sore breasts. Mood swings. Irritability. Cramps. Fatigue. Trouble sleeping. Bloating. Food cravings. Acne. PMS is not kind.
PMS, or premenstrual syndrome, is a set of physical and emotional symptoms that many women suffer from in the days before their periods. These typically appear within the 5 days before menstruation and can last up to a week. The selection and intensity of symptoms vary.
Do I have PMS?
The clinical manifestations of premenstrual syndrome vary and there is no known cause, frustrating physicians and suffering women alike. The intermittent nature of the symptoms does not allow for easy diagnosis, especially since descriptions are not always precise.
As with other bodily processes related to the monthly cycle, consistently recording symptoms and their changes is helpful in assessing the frequency, timing, and severity of the manifestations of PMS. Sometimes women are surprised to find that their symptoms do not seem to track with the changes of their hormonal cycles.
Attention! Certain experiences characteristic of premenstrual syndrome overlap with symptoms of other processes and conditions. If your symptoms are severe, visit your doctor.
For example, your doctor may recommend thyroid testing. Thyroid disorders are common in women of childbearing age, and symptoms such as weight gain, depression, and fatigue may be indicative of thyroid disorder.
Symptoms of PMS can be roughly divided into three categories:
- Physical—hypersensitivity, headaches, breast pain and swelling, joint aches.
- Psychological/emotional—mood swings, signs of depression, irritability, fatigue, sleep disorders.
- Digestive—abdominal swelling, nausea, diarrhea or constipation, vomiting, eating disorders.
PMS or PMDD?
Premenstrual dysphoric disorder (PMDD) is a severe form of PMS. The symptoms of PMDD are similar to those of PMS but are intense enough to interfere with work, social activities, and relationships. PMDD also lasts longer than PMS—up to two weeks.
Symptoms of PMDD include those of PMS as well as additional symptoms, such as fits of temper, decreased interest in usually enjoyable activities, and feelings of hopelessness. Many women with PMDD require medication, however other conditions that could account for these symptoms should be ruled out before diagnosis, including emotional disorders such as depression or panic disorder, and physical conditions such as menopause, endometriosis, fibroids, or hormonal problems.
What causes PMS?
No mechanisms responsible for PMS have been identified, although specialists think that it’s a chemical/neurobiological problem due to cyclic changes in levels of the ovarian hormones, estrogen and progesterone.
By modulating the function of certain brain chemicals called neurotransmitters (such as dopamine and serotonin), these hormones cause changes in mood. Studies have shown that women with mood disorders, depression, and postpartum depression are at higher risk of experiencing PMS.
In combination with low magnesium and calcium levels, the effects on the neurotransmitters may cause an increase in appetite and cravings for specific foods, often for dairy products and sweets.
Swings in estrogen and progestin levels may affect other hormones too, such as aldosterone, which regulates the balance between salt and water. Excessive aldosterone levels can cause water retention and abdominal bloating (a.k.a. meteorism), tender breasts (a.k.a. mastalgia), and weight gain. Depression, withdrawal, insomnia, forgetfulness, and confusion can also occur due to oscillations in our hormone levels.
Research has found that women who suffer from PMDD have a different genetic makeup resulting in a “dysregulated cellular response” to estrogen and progesterone. Studies are ongoing, and there is hope for improved treatment of both PMS and PMDD.
How is PMS treated?
Even with overwhelming evidence of real, physical symptoms, many doctors are still not sure how to treat PMS, and views on different types of therapy are conflicting. The goal of treatment is to relieve symptoms. It starts with a thorough evaluation of PMS manifestations, as well as their impact on functioning in daily life and vice versa.
PMS education & tracking
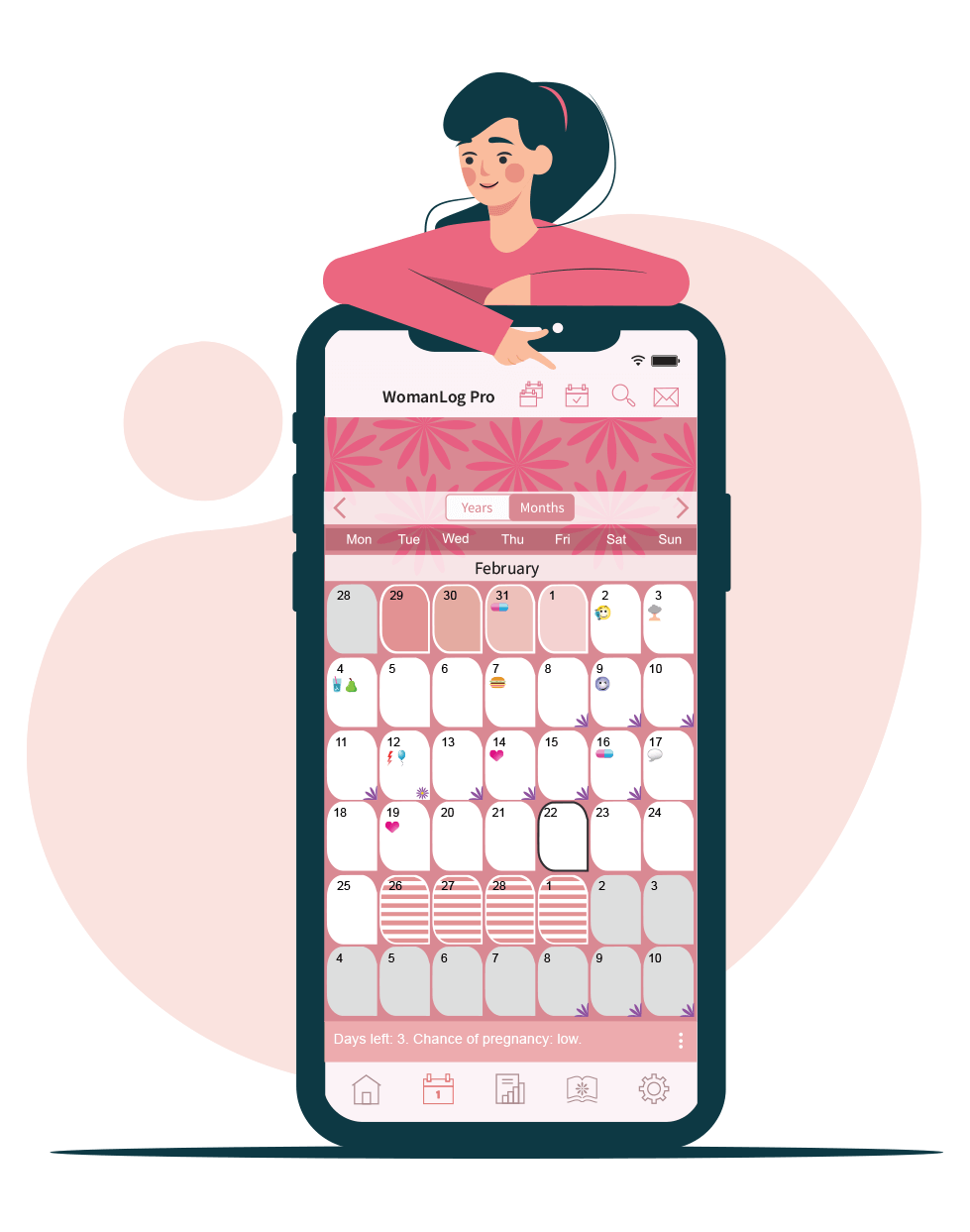
An informed woman will be better equipped to deal with her PMS symptoms than one who cannot identify her aches and pains. A “PMS diary” can paint a more precise picture of the way the body behaves under different conditions, e.g. what a woman experiences during the different phases of her monthly cycle.
Stress relief is also considered effective treatment, especially for women who live a fast-paced life. It’s important to take a breather from your responsibilities from time to time, and to spend time doing things purely for the sake of enjoyment. After consistently dedicating a few days to yourself each month, you may find your symptoms reduced.
For some, breaking out of stressful cycles can be difficult without outside help. In cases of severe anxiety, irritability, or depression, it may be a good idea to seek counseling.
Medication
Over-the-counter painkillers, such as ibuprofen or aspirin, may help relieve cramps, aches, and breast tenderness. Medications may be prescribed in cases of disruptive depression or anxiety. Birth control pills and other hormonal contraceptives can also help by regulating hormonal fluctuations.
Attention! Don’t use over-the-counter painkillers if you suffer from peptic ulcer disease or kidney disease. Doing so, you risk worsening your condition.
A healthy diet is important for your general well-being, including healthy hormone production. Eating balanced meals, reducing your salt, sugar, caffeine, and alcohol intake, and staying well hydrated can help relieve symptoms of PMS.
A number of supplements are often used to relieve symptoms, such as calcium, magnesium, and omega-6. Studies show that not all supplements impact your body as advertised, so consult your doctor about the safety and effectiveness of any supplements you plan to take. Vitamin E and B6 supplements are usually discouraged due to concerns about adverse side effects.
Physical activities can help relieve cramps and bloating in particular. Light exercise, like jogging, releases endorphins, and can help reduce breast tenderness, fluid retention, and depression. Procedures that focus on relaxing your body can reduce anxiety and may temporarily alleviate depression and perceived pain. Perhaps a soothing massage?
You can track your period using WomanLog. Download WomanLog now: