Non-Hormonal Birth Control
Hormonal birth control doesn’t work for all women—some experience side-effects, others just aren’t comfortable with the idea of altering their bodies in such a fundamental way. These are the alternatives.
Non-hormonal birth control includes barrier and natural methods, the copper IUD, and sterilization. The only contraceptives that provide effective protection against STDs are male and female condoms. Unless there is 100% certainty that all participants are 100% STD-free, a condom must be used during sexual intercourse.
Barrier methods
Barrier contraceptives keep sperm from entering the uterus and fertilizing the egg. In general, barrier methods are less effective but have fewer side effects than hormonal methods or IUDs. Barrier methods include condoms, diaphragms, cervical caps, and contraceptive sponges.
The male condom is a thin, flexible sheath-shaped polyurethane or latex barrier that is rolled onto an erect penis before intercourse. When left in place during sexual intercourse, oral sex, or anal sex, male condoms are an effective method of protection against sexually transmitted diseases (STDs, also known as STIs) and pregnancy, since it blocks sperm from entering the vagina.
Condoms are simple to use, inexpensive, and widely available without prescription, and some organizations even hand them out for free. They are made in a variety of lengths, shapes, and colors, and are sold in both lubricated and non-lubricated varieties. Some condoms are textured to increase the sexual pleasure of both partners.
For individuals with a latex allergy, condoms can cause rashes, hives, itching, and a runny nose but there are non-latex options made of polyurethane.
The female condom is a thin, flexible sheath-shaped synthetic nitrile or latex barrier with a ring on each end.
The ring at the closed end is inserted and pushed up to the cervix. The ring at the open end remains just outside the vagina.
The female condom is immediately effective, protects against STDs, and is 95% effective if used properly. It is available without a prescription or special fitting.
The female condom doesn't work for every woman, as some women aren't comfortable with the insertion process or find the outer ring cumbersome.
The contraceptive diaphragm is a round, dome-shaped reusable barrier with a firm, flexible rim. Made of rubber or silicone, it fits inside the vagina and covers the cervix to block sperm from reaching the egg cell. The diaphragm should always be used with spermicide and must be left inside the vagina for at least 6 hours after intercourse but no longer than 24 hours in total. When used correctly, the diaphragm is 92–96% effective.
The cervical cap is also reusable and very similar to the diaphragm. It is made of rubber and shaped like a large thimble. It fits tightly over the cervix, is held in place by suction, and has a strap to help with removal. The cervical cap is effective at preventing pregnancy only when used with spermicide and should be left inside the vagina for at least 6 hours after intercourse but no longer than 48 hours in total.
Both the diaphragm and the cervical cap are not recommended during menstruation, after recent cervical surgery, in case of sensitivity to spermicide, infection, or in the case of an unusually shaped cervix.
The contraceptive sponge is soft, disc-shaped, and made of polyurethane foam. It contains a spermicide that must be activated with water before insertion. In the 24 hours after insertion, the sponge effectively prevents sperm from reaching the uterus. It should be left inside the vagina for at least 6 hours after intercourse but no longer than 30 hours in total.
Non-barrier methods
The copper IUD or intrauterine device is a T-shaped device that is placed inside the uterus and regularly releases a small amount of copper, which acts as a spermicide. The IUD is effective immediately and can last for 5–10 years, depending on type. After removal, chances of getting pregnant return immediately.
Some women experience longer and more painful menstrual periods in the first 3–6 months after having an IUD fitted. There is some risk of infection, and of your body pushing the device out—your doctor will let you know how to check if it’s in place. The IUD is not recommended for women who are pregnant or have a history of pelvic infection.
Natural methods
Natural birth control methods are those that rely entirely on being attentive to what’s going on in the body—by controlling male ejaculation during sex, reading bodily signs that indicate whether a woman is ovulating, or both. Although generally less effective than other methods, natural methods are better than nothing, and are more accepted within some religious beliefs.
The withdrawal method (“coitus interruptus” in Latin) is the practice of withdrawing the penis from the vagina before ejaculation. As an easily available and free birth control method with no side effects, it’s quite convenient.
Still, it has its downsides:
- First, it isn’t all that reliable. Semen may enter the vagina if withdrawal isn't properly timed or if the pre-ejaculate fluid, or precum, contains sperm.
- Second, natural methods don't offer any protection against STDs.
- Third, it requires considerable concentration and self-control. This can make it difficult to enjoy sex, as having to be conscious of timing one’s actions can be stressful and sex must be interrupted at the height of pleasure. An unhealthy approach to this method can become a psychological barrier for either or both partners, which may cause relationship problems.
The cervical mucus method is a type of natural family planning considered a fertility awareness-based method. Success relies on careful observation of mucus patterns during the menstrual cycle. Cervical discharge changes over the course of the monthly cycle. By recognizing the changes of her cervical mucus, a woman can predict when ovulation will occur and determine when she’s more likely to conceive, avoiding unprotected sex during that time.
This method requires keeping a close eye on the body and recording all changes. It carries some risk of hampering the sex life of partners involved due to lack of spontaneity. Doctors estimate that the cervical mucus method is typically about 77% effective during the first year, but can be up to 97% effective if used correctly.
The cervical mucus method is sometimes combined with another method of natural family planning such as tracking basal body temperature, as a woman's temperature naturally rises during ovulation, or the calendar method.
The calendar method or rhythm method is another form of natural birth control. Just as with the cervical mucus method, a woman tracks her menstrual cycle to predict when she will ovulate and avoids unprotected sex during that time.
The calendar method also requires careful record keeping and persistence, and bears no cost or health risk. The calendar method is estimated to be 80–87% effective on average.
The lactational amenorrhea method, or LAM, is only effective during the first 6 months after giving birth and involves nothing but breastfeeding. Breastfeeding suppresses a woman’s fertility as long as her period has not returned and her baby is feeding on demand without any supplemental foods or liquids.
Sterilization
Sterilization is an option for both men and women who no longer wish to have children. Although effective against pregnancy, it offers no protection against STDs.
Tubal ligation, also known as having one’s tubes tied, is a type of permanent birth control for women. The fallopian tubes are surgically tied, blocked, or cut. Most tubal ligation procedures are irreversible. Reversal may be attempted in some cases, but this requires complicated surgery and isn't always effective.
The procedure doesn't affect the hormonal system or menstrual cycle—and there is still a small risk of ectopic pregnancy in which a fertilized egg implants outside the uterus, usually in one of the fallopian tubes. An ectopic pregnancy is a potentially dangerous condition that requires immediate medical treatment.
However, tubal ligation is generally considered safe, and may decrease the risk of ovarian cancer, especially if the fallopian tubes are removed.
Vasectomy is surgical contraception for men. The vas deferens, or tubes that carry sperm, are cut and sealed so that no sperm can enter the semen. Vasectomy is considered a safe, but irreversible form of birth control. If a man does want to father a child following sterilization he can turn to in vitro fertilization or adoption.
Sterilization is a serious decision for either sex and should be considered carefully. Some people disagree with these procedures entirely, but remember that your body is your own and what you do with it is no one’s business but your own.
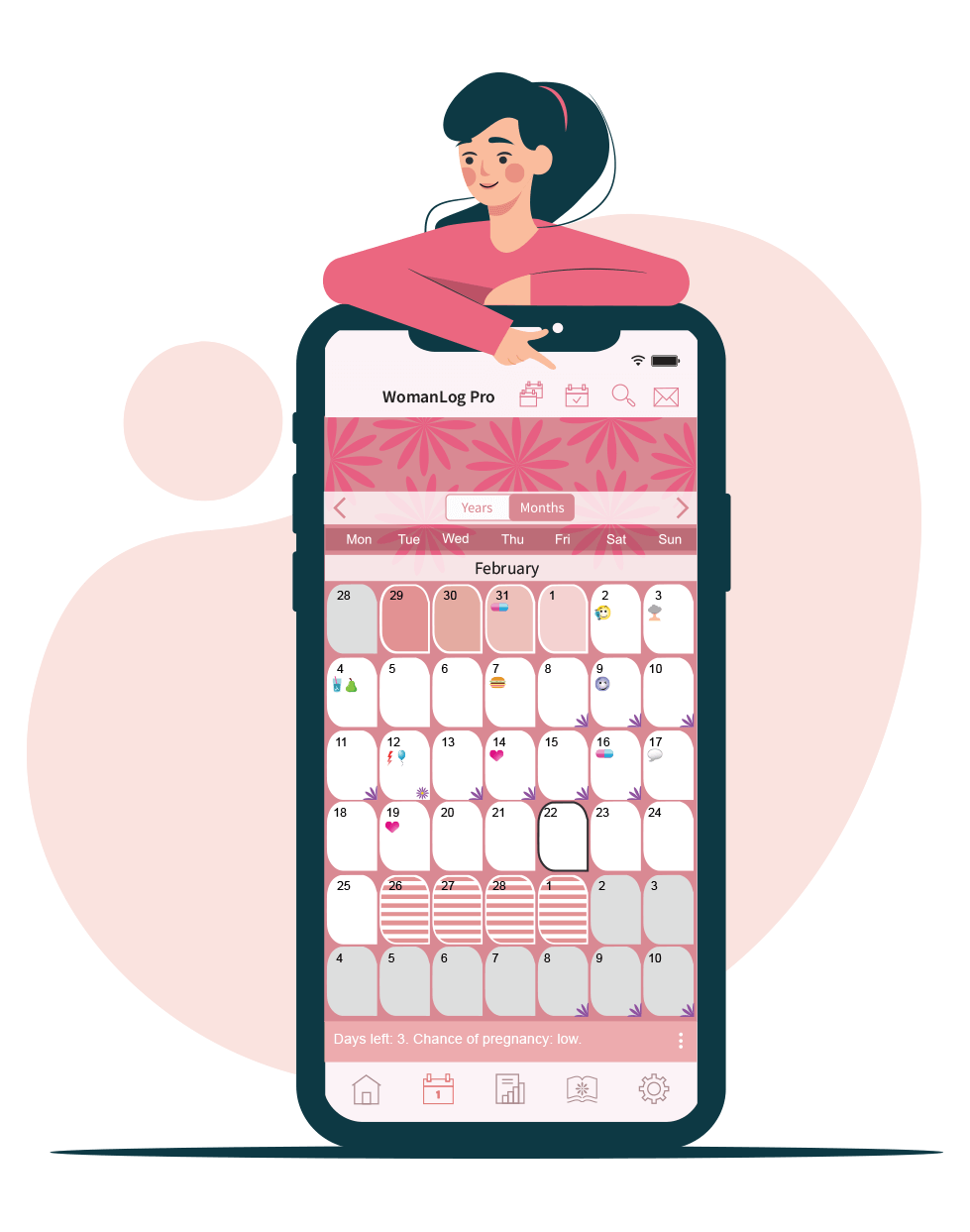
You can use WomanLog for non-hormonal birth control. Download WomanLog now: